Preventing the development or delaying the progression of type 1 diabetes (T1D) could significantly improve long term health outcomes for those potentially affected by the disease. To make this vision a reality, we fund research to better understand the disease, identify those at risk or in early stages of the disease, and discover and test new therapies.
Understanding the Disease
We support scientific research to better understand the human disease to design, develop, and select therapies with the highest potential impact.
Supported projects include research into human genetics in T1D, and factors that protect an individual from the development of T1D.
Screening for Early-Stage Disease
Early-stage disease detection can prevent hospitalizations at diagnosis, improve long-term health outcomes, allow earlier care decisions, facilitate participation in clinical trials, and enable treatment with approved therapies. Screening for T1D-related autoantibodies can identify people with early-stage disease, who will later develop clinical T1D, sometimes years before they have symptoms and need insulin, but this kind of screening is not widely available.
To realize the short- and long-term benefits of early detection, monitoring, and early treatment Helmsley-funded projects seek to generate evidence for the adoption of islet autoantibody screening as part of routine pediatric care. While relatives of people with T1D are at significantly increased risk of developing the condition, most people who develop T1D do not have an affected relative, so Helmsley supports projects aimed at developing this screening for the general population.
Developing New Therapies, From Discovery to Trials to People
We support the discovery and testing of new therapies that have the potential to prevent or delay the onset of clinical T1D, and to improve the lives of people with T1D.
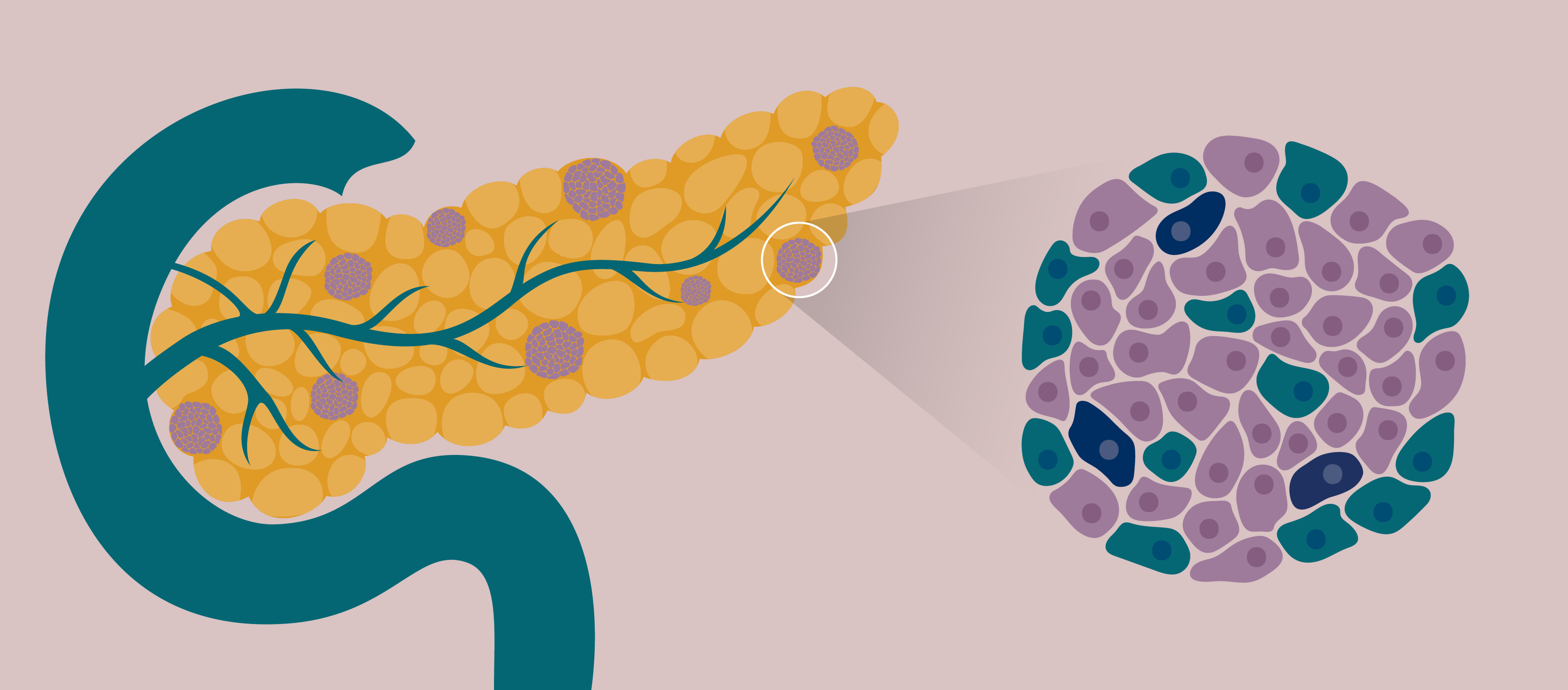
Preventing T1D requires developing therapies that deter the autoimmune attack on the body that destroys the insulin-producing beta cells in the pancreas. Identifying prevention therapies is a long-term endeavor fraught with challenges, yet promises great reward.
We support advancement from basic biological discovery, to preclinical development, to clinical testing. By helping therapies get closer to the final testing stages and tackling field-wide barriers to T1D drug development, we aim to ensure that promising, potentially transformational therapies are not left on the drawing board due to the high risks of failure associated with drug development.
Supported projects include research into targeted immunotherapies, preventing hypoglycemia, and improving metabolic control.
Through our work, we encourage and facilitate collaboration and knowledge exchange among investigators working on related topics to enhance and accelerate research efforts. We support large-scale, collaborative efforts that are essential for both clinical research and clinical trials, and research into therapies that might not get off the ground without philanthropic funding. Our goal is to create a clear path from initial discovery to the hands of people with T1D.