One aim of the Crohn’s Disease Therapeutics pillar is to identify top researchers whose findings may lead to new medications for the treatment of Crohn’s disease. When thinking about medication, a quick image that comes to mind is usually a pill or capsule containing a chemical providing a beneficial effect. Medicine, however, is not limited to pills. Many drugs are creams, fluids, or even whole cells – as in a blood transfusion or bone marrow transplant. As with almost any treatment, using cells as a therapeutic may have certain risks, but specific cell types may have unique beneficial effects which could prove to be the next frontier in treating Crohn’s disease.
Most people are familiar with blood transfusions and, in fact, donating blood can be one of the easiest ways to save a life. Donated blood contains many cell types, including red blood cells which carry oxygen, white blood cells which mediate immune responses, and platelets which are necessary for blood clotting and wound healing. Heterologous donations, those that come from another person, must be matched to the donor (such as blood type ABO matching).
Since blood cells do not multiply and have a limited lifespan, blood transfusions provide only temporary effects. Bone marrow transplants, on the other hand, can have lasting, even lifelong, effects. This is due to the presence of stem cells within the bone marrow which can mature into all types of blood cells and are self-renewing to make even more stem cells. In this way, a bone marrow transplant can replace not only the red blood cells of an individual but their immune system as well. This carries the risk that the new immune system will see the host as foreign and attack it (a condition known as graft versus host disease) and requires that the donor bone marrow be as closely matched to the recipient as possible.
In recent years, cell-based therapies have expanded beyond blood and bone marrow, focusing on other cell types, and even reprogramming cells outside the body before returning them to the host. As a current area of cutting edge therapeutics, the Crohn’s Disease Program has given multiple grants to support research in this space.
Two of these grants, focus on the use of a particular type of stem cell, mesenchymal stem cells (MSCs), that can give rise to bone, muscle, and connective tissue. These cells are most commonly isolated from fat tissue or bone marrow and present a low profile to the immune system, reducing the risk of rejection and the need for the donor to be matched to the recipient. In addition, MSCs have been shown to speed healing and provide anti-inflammatory effects.
Dr. Alyssa Parian and colleagues at Johns Hopkins University (JHU) have been studying MSCs to aid in the repair of perianal fistulas, a devasting complication of Crohn’s disease where channels open between the rectum and the surrounding tissue, leading to infections and incontinence. The group at JHU has developed animal models to study fistula healing using stem cells from both placenta and fat tissue. They have treated their first patients with promising results and recently opened a Center of Excellence for the treatment of perianal fistulas.
Similarly, Dr. Amy Lightner and colleagues at the Cleveland Clinic are testing MSCs for the treatment of fistulas. These MSCs, derived from bone marrow of healthy donors, are isolated and prepared for injection at Cleveland Clinic and have been used to treat 60 patients to date with encouraging results. The team recently received additional Helmsley funding to double the number of patients enrolled. They will also be collecting tissue from the patients before and after treatment to better understand how the tissue is healing in response to the MSC transplant.
Another grantee, Dr. Louis Cohen at the Icahn School of Medicine at Mount Sinai (ISMMS), is also studying stem cells. Instead of using donor cells, he is studying autologous transplantation – giving patients back their own bone marrow after chemotherapy in an attempt to “reset” the immune system. While earlier trials with autologous stem cells showed some promise in treating patients who were not responsive to any other medications, the remission achieved by these patients was temporary. Dr. Cohen and his colleague Dr. Judy Cho hypothesize that an autologous transplant, followed by proactive treatment with a biologic drug (vedolizumab) that is approved for treating Crohn’s disease, could increase the durability of remission. They are also conducting research to explore whether genetic risk factors for Crohn’s disease that may be present in stem cells can be corrected, in effect reprogramming the cells before they are returned to the patient.
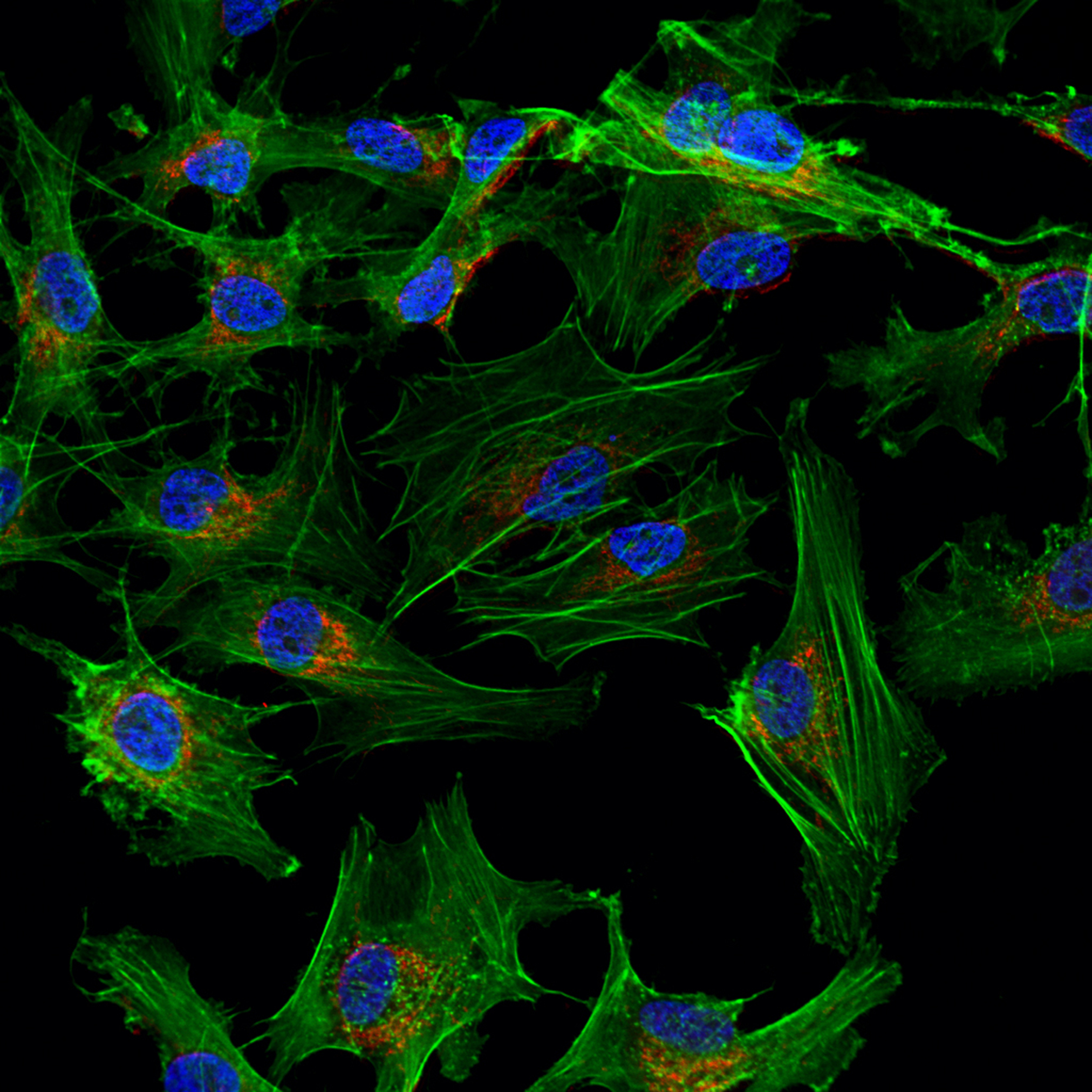
Dr. Derek McKay at the University of Calgary is also exploring manipulation of patient cells in the lab for enhanced therapeutic potential. In this project, the investigator and his colleagues are focused on macrophages, a type of white blood cell that resides in tissues and serves as an early detector of infectious invaders. A subtype of macrophages, termed M2, specifically play a role in dampening down and resolving inflammation after an infection has been cleared. Dr. McKay has developed a protocol to isolate macrophage precursor from the blood and induce them to become M2 macrophages. He hopes to isolate patient cells, treat the cells to become M2 macrophages, and then return the new M2 macrophages to the patient to ameliorate the inflammation in Crohn’s disease.
While more complex than traditional medicinal approaches, cell-based therapies are an innovative and promising area for exploration. The Therapeutics team within the Crohn’s Disease Program is excited by the success of our grantees to date and we look forward to more results as studies continue. We will continue to seek out new grants in this exciting space as we move toward our goals of treating, and someday curing, Crohn’s disease.