The therapeutic goal in Crohn’s disease is to move individuals into remission as soon as possible and for as long as possible. One key challenge is that not every drug works for every patient, and some drugs can lose their effectiveness over time. Helmsley is committed to discovering new interventions and optimizing current therapies to induce and maintain long-term remission through a precision medicine approach -- getting the right drug to the right person at the right time. Everything we do is focused on one question: what is best for the individual patient?
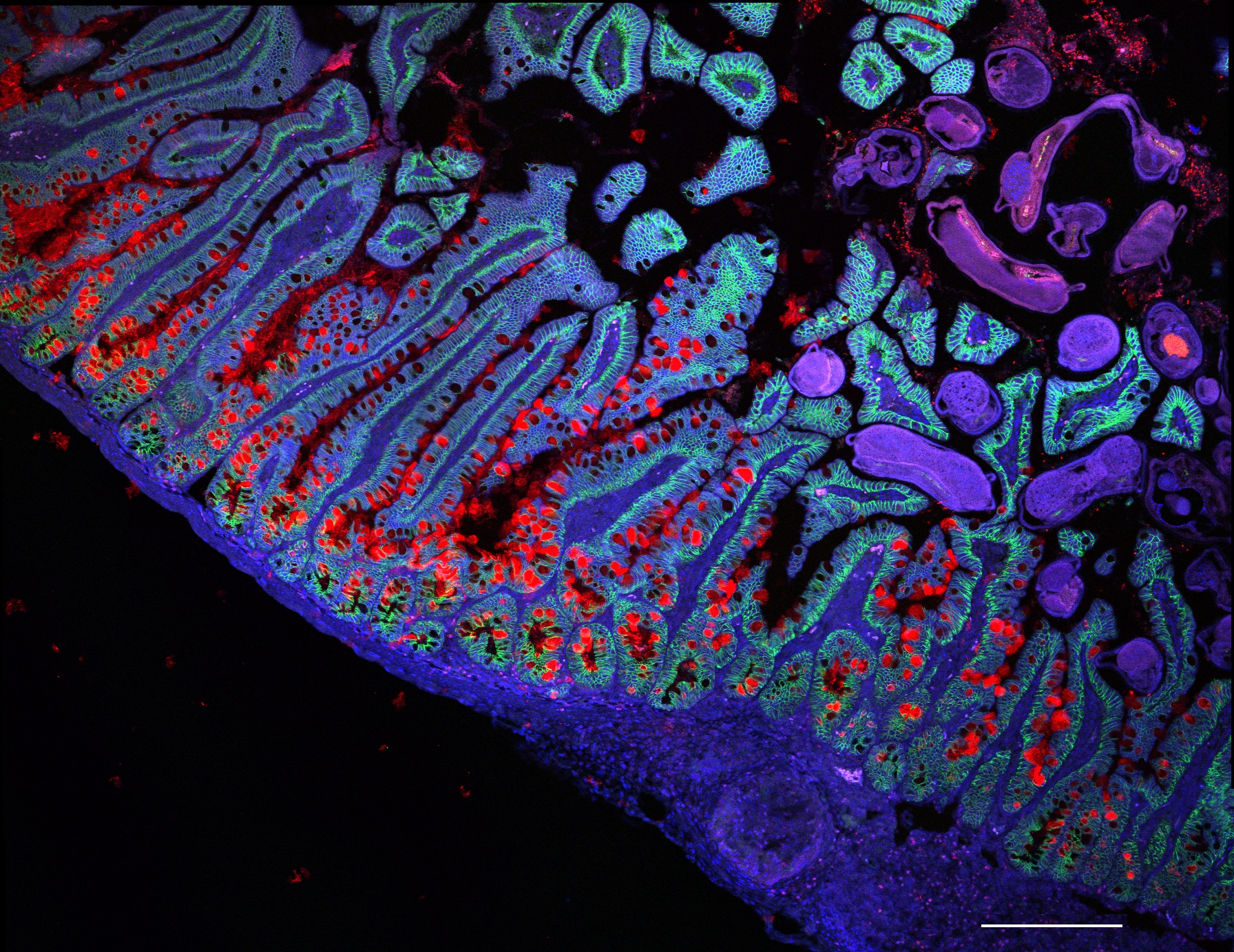
Our research grants are directed toward three therapeutic levers that we believe can achieve these ends – establishing immune homeostasis, addressing microbial dysbiosis, and promoting epithelial healing. Most existing therapeutics involve tamping down the aberrant immune response, and we support research to improve upon and optimize these immune-based therapies. Imbalance of the intestinal microbiome is known to play a role in Crohn’s disease; we support programs that further the understanding of microbial communities and that explore interventions to restore them to a healthier state. We are also focused on the epithelial barrier of the gastrointestinal tract by investigating whether epithelial disruption is a cause or an effect of Crohn’s disease and what treatments can be introduced to restore integrity of the barrier.
Throughout these efforts, we seek to translate insights from animal models to human clinical studies and to accelerate the time to market for novel and innovative therapeutics.
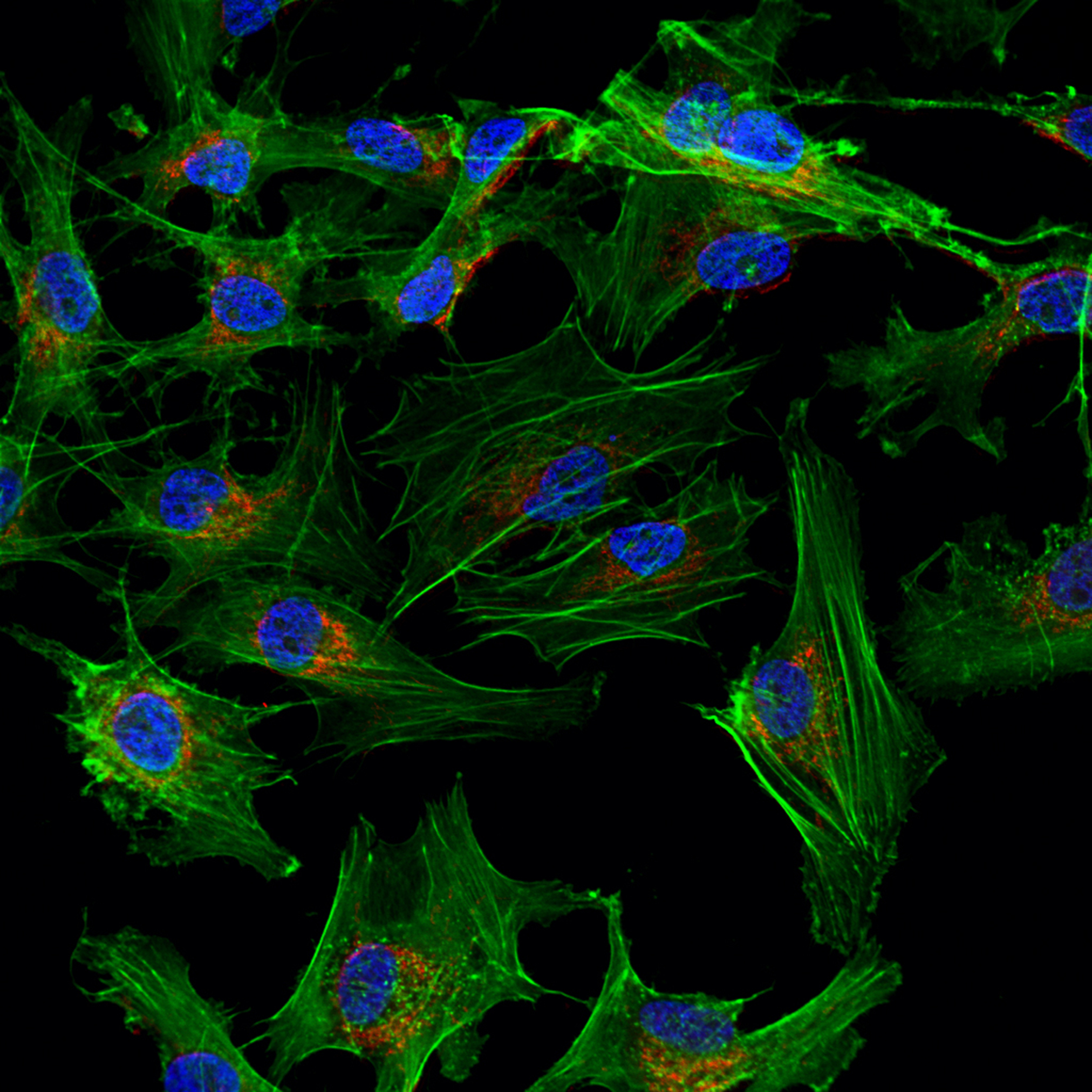
Finally, we acknowledge that our limited understanding of the underlying pathophysiology of Crohn’s disease hampers our ability to develop effective therapeutics. Helmsley is funding the creation of a Gut Cell Atlas, which is cataloging the many cell types in the small and large intestines, yielding insights into the molecular basis of Crohn’s disease and spurring new treatments. This effort is part of a global Human Cell Atlas, which is transforming what we know about human health.