Achieving Equitable Access in Low- and Middle-Income Countries


People living with type 1 diabetes (T1D) in low- and middle-income countries face a 50-year gap in life expectancy compared to those in high-income countries.1 Helmsley’s T1D global access portfolio works to address this stark inequity by ensuring that people living with T1D have medicine in hand and access to care, when and where they need it. For all people with T1D, access to affordable medicines and health supplies can be the difference between life and death.
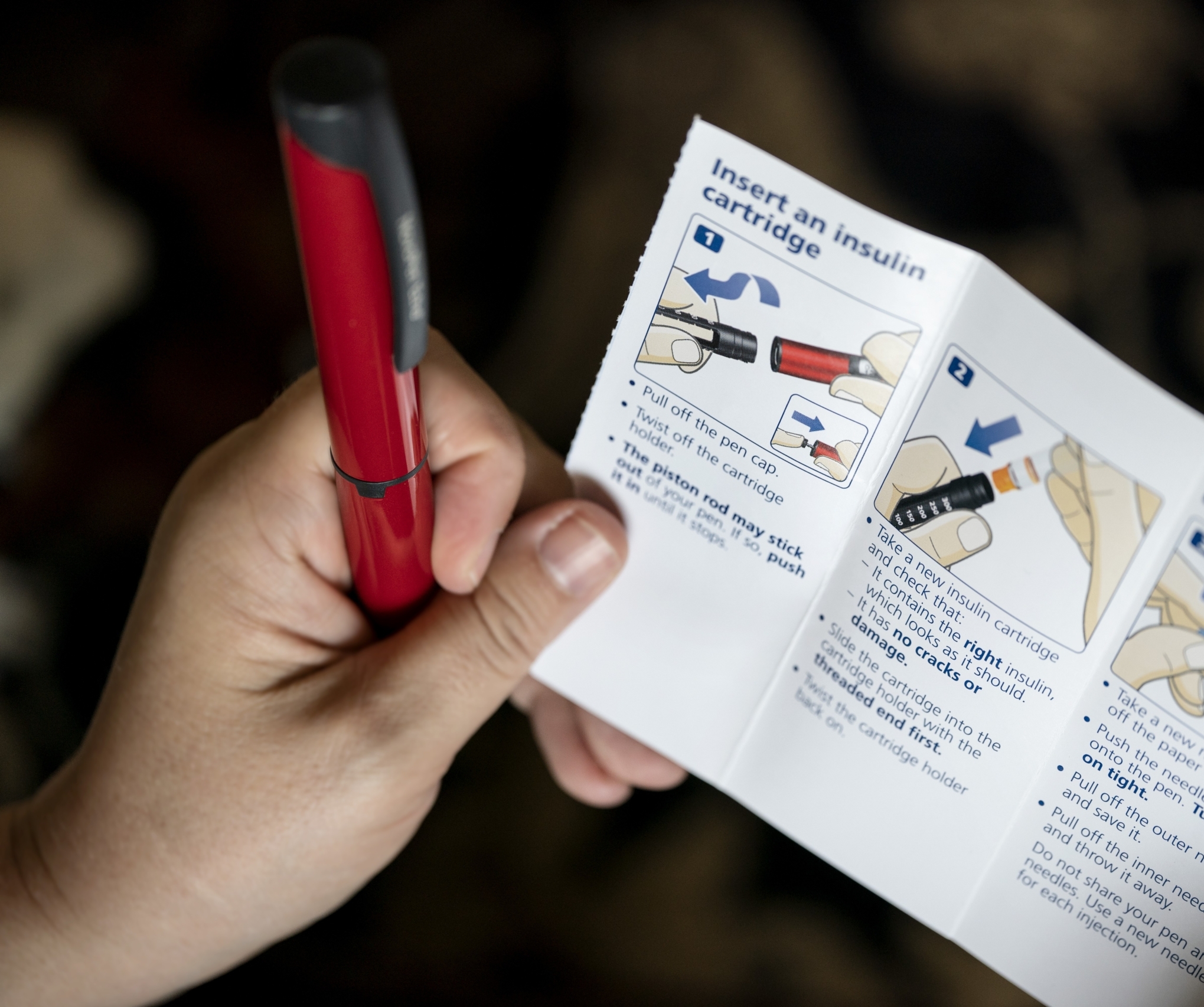
We are working to address the immediate, urgent needs to increase access to insulin and other life-sustaining supplies through support for donation programs and T1D clinics. At the same time, we are working to establish lasting, long-term solutions. We support efforts to expand integrated care models, to shape commercially sustainable markets for medicines, and to build a global movement to treat chronic noncommunicable diseases, such as T1D.
Helmsley is committed to breaking down partner silos, building coalitions, and investing in community-led solutions. By taking bold risks and forging deep, long-term partnerships rooted in a shared vision, we can dismantle deeply entrenched barriers and help build a world where everyone can live full, healthy lives — no matter the diagnosis, no matter where they call home.
1 Gregory, A. G. (Oct 2022). The Lancet: Diabetes & Endocrinology. “Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with a projection to 2040: a modelling study.” Download here.

June 9, 2025
May 13, 2025

August 19, 2024

June 25, 2024

December 8, 2023

October 25, 2023
December 18, 2023
Recognizing the critical need for access to quality diabetes care in humanitarian settings, The Leona M. and Harry B. Helmsley Charitable Trust today announces a $2.6 million grant to the International Alliance for Diabetes Action (IADA) to address diabetes within the context of rising global displacement.
November 15, 2023
Every year on November 14 — World Diabetes Day — Helmsley partners with the Empire State Building and the Helmsley Building to light the New York City skyline blue and raise awareness about type 1 diabetes. As we reflect on this day where the diabetes community comes together to envision a brighter future, we’re inspired by our grantees working to…
September 23, 2023
NEW YORK, September 21, 2023 — The Leona M. and Harry B. Helmsley Charitable Trust today announced a US$3 million grant to support the Global Polio Eradication Initiative (GPEI) and protect children around the world from polio. Polio is a devastating, life-threatening, yet vaccine-preventable disease. In 1988, over 1,000 children were paralyzed by the poliovirus across 125 countries every single…
July 20, 2023
At the 2023 World Health Assembly, leaders from across the globe came together to discuss the most pressing issues in health. Helmsley hosted Advancing Equity: Global Action for People Living with Diabetes, a panel event focused on the Global Diabetes Compact (GDC), the World Health Organization’s framework for aligning governments, private businesses, civil society, and people with lived experience to…
July 18, 2023
Following two recent grants to World Health Organization Global Diabetes Compact and the World Health Organization’s Regional Office for Africa, Liz Longley from Inside Philanthropy called Helmsley a “movement builder” in the “high stakes race to manage noncommunicable diseases (NCDs)” in low- and middle-income countries. Global barriers to equitable healthcare are deeply entrenched, but Helmsley is working with many partners to…
June 28, 2023
The Leona M. and Harry B. Helmsley Charitable Trust today announced a US$9 million grant to the World Health Organization (WHO) Regional Office for Africa to expand care for people living with severe noncommunicable diseases (NCDs) in sub-Saharan Africa.